“The risk of a DVT occurring on a flight lasting more than four hours is between 1 in 4,650 flights and 1 in 6,000 flights.”
Your lungs have many functions in your body beyond just oxygenating your blood. One of their other important roles is filtering the venous blood that returns from the body. The venous system is characterized by slower blood flow than the arterial system, which contributes to the occasional formation of a blood clot (known as a “peripheral venous thrombosis”), which could be transported into the lungs and could even cause a pulmonary embolism (or blockage in the vessels of the lungs).
In this chapter, you’ll learn about:
Deep Vein Thrombosis
Deep vein thrombosis (DVT) is a condition in which a blood clot (a “thrombus”) forms in one or more of the body’s deep veins, usually in the legs. If a clot breaks free and travels through the circulatory system, it can lead to life-threatening conditions. For example, if a clot lodges in the lungs, it is known as a pulmonary embolism (PE) and affects the lungs’ ability to oxygenate the blood (see “Pulmonary Embolism”). Collectively, DVT and PE are sometimes referred to as venous thromboembolisms (VTEs).
A clot that originates as a DVT can also cause a stroke in individuals with a patent foramen ovale (PFO, a hole in the wall between the atria — see “Patent Foramen Ovale” for details about this condition); in such a case, the clot travels through the veins to the right atrium of the heart, passes through the PFO to the left atrium and then travels through the arteries to the brain.
DVT is not related to diving, but divers often travel, and travel is a significant risk factor for DVT. In about half of all cases of DVT, the individual experiences no noticeable symptoms before the onset of the condition. Most often, it starts in the calf. Symptoms may include the following:
- Swelling in the affected leg, ankle or foot
- Pain in the calf that spreads to the ankle or foot
- Warmth in the affected area
- A change in the color of the skin — to pale, red or blue
Most VTEs related to air travel occur within two weeks of the flight and are resolved within eight weeks. If untreated, a DVT that starts in the calf will spread up into the thigh and pelvis in about 25 percent of cases. An untreated DVT of the thigh and pelvis has about a 50 percent risk of leading to a PE, which is the most serious complication of DVT. Many cases of DVT are asymptomatic and resolve spontaneously. However, DVT often recurs in an individual who has had one episode of the condition.
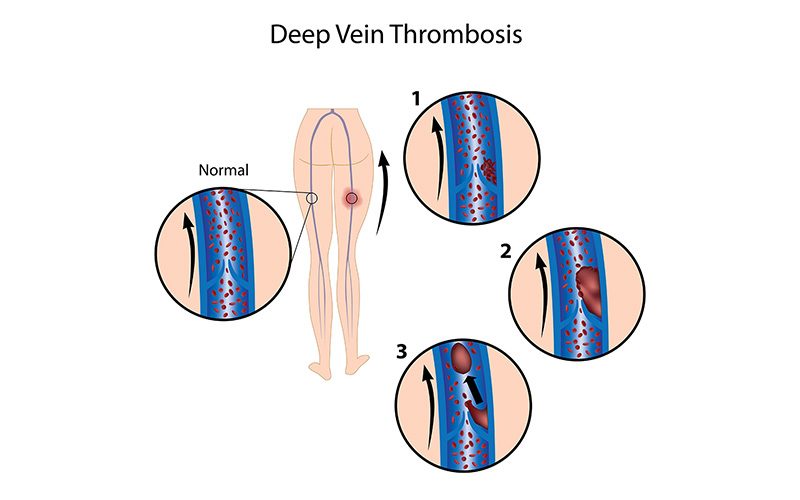
Most DVTs occur in individuals with pre-existing risk factors for DVT who remain motionless for a long time — such as when traveling a long distance by plane, car or train; when doing deskwork over a period of many hours; or when bedridden. This is because immobility slows down the blood flow in the veins (a condition known as “venous stasis”); in addition, pressure on the calf from an inadequate seat can injure the vein walls. If you sit still for 90 minutes, the blood flow in your calf drops by half, and that doubles your chance of developing a blood clot. For every additional hour you spend sitting, your risk of a blood clot increases by 10 percent.
The incidence of DVT in the general population is one-tenth of one percent, but it is higher in those who have risk factors and those who travel often. Long-distance air travel may double or even quadruple the risk of suffering a VTE. Although DVT is often called the “economy class disease,” business-class travelers are susceptible, too. The risk of a DVT occurring on a flight lasting more than four hours is between 1 in 4,650 flights and 1 in 6,000 flights; this is lower than the risk in the general population, but that’s because people who take long trips are likely to be healthier than average. The incidence of DVT among travelers with a low to intermediate pre-existing risk for VTE who take a journey longer than eight hours was found to be 0.3 percent for symptomatic cases and 0.5 percent when including asymptomatic cases as well.
Risk factors for DVT include the following:
- Older age (the risk rises after age 40)
- Obesity (defined as a body mass index greater than 30)
- Estrogen use (either hormonal contraceptives or hormone replacement therapy)
- Pregnancy (including the postpartum period)
- Thrombophilia (an abnormally increased tendency of the blood to clot)
- Previous VTE or a family history of VTE
- Active cancer
- Serious medical illness
- Recent surgery, hospitalization or trauma
- Limited mobility
- Central venous catheterization (the presence of a catheter in one’s chest, for use in administering medication or nutrients and/or drawing blood samples)
Between 75 percent and 99 percent of those who develop a travel-related VTE had more than one of these risk factors.
Height is also a factor in one’s risk of developing a travel-related DVT. People who are either very short — less than 5 feet, 3 inches (1.6 meters) — or very tall — more than 6 feet, 3 inches (1.9 meters) — appear to be at increased risk as a result of their inability to adjust their seats sufficiently to accommodate their height. In addition to effects of immobility, shorter passengers may suffer greater than usual seat-edge pressure on the backs of their knees, and taller passengers may be cramped due to insufficient leg room. All of these factors can contribute to injury of deep veins, venous stasis and activation of the blood’s clotting mechanisms.
Those who are at increased risk of DVT should wear compression socks whenever they fly or drive long distances and should consult their primary-care provider regarding the possible benefit of taking a clot-preventative such as aspirin. Although the risk of DVT for healthy people is small, everybody should be aware of the factors that can precipitate the condition — and avoid long periods of immobility. The best way to prevent DVT is to get up and walk around from time to time. It also helps to flex your feet and calf muscles regularly if you must remain seated for any length of time. Finally, it is also helpful in preventing DVT to stay well hydrated.
Effect on Diving
Any individual who has been diagnosed with acute DVT or who is taking anticoagulants should refrain from diving. It may be possible to return to safe diving after having a DVT, but the evaluation of fitness to dive must be made on an individual basis.
Pulmonary Embolism
A pulmonary embolism (PE) is an obstruction (or “embolus”) that lodges in the vasculature of the pulmonary system, or lungs. The embolus may be air, fat or a blood clot (or “thrombus”). If a PE is caused by a thrombus, the clot typically originated in the deep vein system of the legs — a condition known as deep vein thrombosis (DVT); see “Deep Vein Thrombosis” for a discussion of DVT. The resulting obstruction in the flow of blood to the lungs typically causes a drop in cardiac output and a significant drop in blood pressure.

The onset of PE can be acute or chronic. Acute PE often causes symptoms evident to the individual, while chronic-onset PE frequently reveals its presence only with very subtle findings that went unnoticed by the affected individual. An untreated PE has a high mortality rate. An especially grim prognosis applies to individuals who have a concurrent DVT, right ventricular thrombus or right ventricular dysfunction. An estimated 1.5 percent of all deaths are diagnosed as being due to PE.
Risk factors for DVT — and thus for PE — include recent surgery; a stroke; a diagnosis of autoimmune disease, malignancy or heart disease; obesity; smoking; hypertension; and a previous DVT.
Symptoms of PE include chest pain (also known as “dyspnea”), pain or swelling of the calf (signaling a DVT), hypotension (abnormally low blood pressure), an altered level of consciousness and syncope (fainting). Distension of the neck veins in the absence of other conditions — such as pneumothorax (a buildup of air in the membrane surrounding the lungs, sometimes referred to as a collapsed lung) or heart failure — may also be observed in individuals suffering a PE.
PE should be one of the first conditions considered when attempting to make a diagnosis in someone exhibiting acute onset of any of the symptoms listed above and any of the associated risk factors. Appropriate diagnostic tests may include measurement of the individual’s levels of a hormone called brain natriuretic peptide (BNP) and of a protein known as cardiac troponin, as well as a CT angiogram of the lungs.
Treatment should focus initially on managing the significant cardiopulmonary impairments that are usually involved in a PE. Such care may include breathing support from an artificial ventilator and fluid management. The use of anticoagulant medication is also important, both to treat the embolus and to stop the development of another thrombus. Thrombolysis (known as “clot-busting”), embolectomy (surgical removal of the embolus) or the placement in the vena cava (one of the large vessels in the chest) of a filter designed to prevent any future clots from reaching the lungs may also be considered — especially in anyone who goes into shock, because mortality in such cases approaches 50 percent. Similar measures may be called for in cases of PE caused by a venous gas bubble. Hyperbaric oxygen therapy may be indicated as well, if the individual’s condition does not improve or deteriorates even after the application of supportive measures.
Effect on Diving
Despite many medical advances, five-year all-cause mortality in individuals who have suffered a PE due to underlying risk factors remains more than 30 percent. And pulmonary hypertension — elevated pressure in the arteries that carry blood from the heart to the lungs, a condition that limits one’s exercise capacity — often persists in individuals who have had a PE, even after successful treatment. Thus any determination of fitness for diving by those who have had a PE must include an evaluation of their lung function, underlying conditions, anticoagulation status, exercise capacity and cardiac status.
Immersion Pulmonary Edema
Immersion pulmonary edema (IPE) is a form of pulmonary edema — an accumulation of fluid in the tissues of the lungs — that specifically affects divers and swimmers. Immersion at depth is a key factor in the development of IPE. That’s because immersion in an upright position causes a significant shift of fluid from the peripheral to the central circulatory system, resulting in higher pressure in the capillaries of the pulmonary system. Elements of the diving milieu that contribute to IPE’s occurrence include the fact that divers breathe gases that are denser than air at sea level, which means more negative pressure within chest is needed to inhale; the likelihood of gas bubbles becoming trapped in the vasculature of the lungs; the cold underwater environment; and the potential in underwater settings for exertion or panic, which can exacerbate elevated capillary pressure.

Maintaining a proper fluid balance in your lung tissue and its vasculature requires a dynamic combination of various opposing forces. Unopposed changes in any of these forces can result in a buildup of excess fluid — or edema — in your pulmonary tissue. The main variables involved in regulating this fluid balance are the following:
- Oncotic pressure (a form of pressure exerted by proteins) in the pulmonary capillaries, the tiniest vessels of the circulatory system
- Oncotic pressure in the pulmonary system’s interstitial fluid (fluid in the cavities of your lung tissue)
- Permeability of the pulmonary capillaries
- Hydrostatic pressure (the pressure of a fluid at rest) in the pulmonary capillaries
- Hydraulic pressure (the pressure of a fluid that is being compressed or pumped) in the interstitial fluid
- Pressure in the alveoli, the tiny air sacs of the lungs.
These factors, which collectively are known as “Starling forces,” can all be quantified and placed in an equation that can then be used to calculate the net differential of
the forces.
Pulmonary edema is caused by changes in these forces — such as a drop in the levels of key proteins in the blood; leakage from the pulmonary capillaries due to sepsis (a life-threatening complication of infections); an increase in hydrostatic pressure in the pulmonary capillaries due to heart failure; and negative pressure in the alveoli due to resistance from breathing through a faulty regulator. Additional issues that can contribute to the development of pulmonary edema include side effects of some cardiovascular drugs; ARDS (acute respiratory distress syndrome, a life-threatening condition that prevents oxygen from getting to the lungs); reperfusion (a procedure that restores circulation after a heart attack or stroke); cardiomyopathy (a weakening of the heart muscle); high-altitude pulmonary edema; a pulmonary embolus (a blood clot lodged in a vessel in the lungs); re-expansion (the reinflation of a collapsed lung); pulmonary hypertension (elevated pressure in the arteries that carry blood from the heart to the lungs); lung cancer; hemorrhage (uncontrolled bleeding); and various disorders of the nervous system. Other factors can include overhydration by well-intentioned divers who have heard the conventional wisdom that dehydration is a risk factor for decompression sickness, as well as poor physical conditioning, which can result in increased negative pressure in the alveoli during deep inspiration.
The symptoms of IPE include chest pain; dyspnea (discomfort or difficulty breathing); wheezing; and pink, frothy sputum while submerged or shortly after emerging from the water. Most people who suffer an episode of IPE had no significant history or signs that would indicate a susceptibility to the condition; nevertheless, the risk of IPE does rise with age, obesity and elevated blood pressure.
Once pulmonary edema occurs, hypoxia (lack of an adequate supply of oxygen) leads to constriction of the pulmonary vasculature, which worsens the cascade of ill effects. The situation can be further aggravated by the accompanying dyspnea, which, when experienced underwater, can induce panic and uncontrolled ascent to the surface — leading to overinflation of the lungs and even near-drowning.
To help differentiate immersion pulmonary edema from other conditions with similar symptoms (such as near-drowning, pulmonary decompression sickness and pulmonary overinflation syndrome), it is important to keep in mind that IPE’s onset can occur either at depth or upon reaching the surface. And it is not necessarily precipitated by aggressive diving, a rapid ascent or the aspiration of water.
Treatment for IPE should begin with removal of the affected individual from the water (to relieve the compression of the vessels in the lower extremities, allowing centrally pooled fluids to return to the extremities) and with administration of oxygen (beginning at 100 percent and later at a reduced concentration). A diuretic such as Lasix may help to reduce excess intravascular fluid, although diuresis — the body’s natural excretion of fluid — may already be under way as a result of hormonal influences. The condition usually resolves quickly in a healthy diver. Prolonged hospitalization is rarely required; if it is necessary, it’s usually due to contributing factors, such as an underlying cardiac problem.
Effect on Diving
Some divers have one episode of IPE and never experience the condition again, but repeated episodes are likely. Any individuals who suffer a first episode of IPE are advised to undergo a detailed examination to rule out any medical conditions that may have caused the edema and then to have a thorough discussion with their physician regarding the risks of continuing to dive. And all divers are urged to have regular maintenance on their regulators, to refrain from overhydration and to attend to proper dive planning in order to avoid exertion and panic — as well as to keep conditions such as obesity and hypertension under control.
